TL;DR
Stanford researchers report that blocking the age-linked protein 15-PGDH rebuilt knee cartilage in aged mice and prevented osteoarthritis after ACL‑like injuries. Human knee tissue samples incubated with the inhibitor also showed early signs of articular cartilage regeneration; clinical use for joints is not confirmed in the source.
What happened
Scientists at Stanford Medicine published a study in Science showing that a small‑molecule inhibitor of the age-associated protein 15‑PGDH can regenerate joint cartilage in mice and reduce post‑injury osteoarthritis. The team administered the inhibitor systemically and directly into knee joints of aged animals; treated knees thickened with hyaline (articular) cartilage rather than lower‑quality fibrocartilage. In a separate model mimicking ACL injury, injections twice weekly for four weeks markedly reduced the development of osteoarthritis and improved limb use. Analysis showed the drug shifts gene expression in existing chondrocytes—reducing cell populations linked to degradation and fibrocartilage and increasing those tied to hyaline cartilage—without recruiting stem cells. Human knee tissue removed during joint replacement, when treated ex vivo for a week, exhibited reduced 15‑PGDH expression and began forming functional articular cartilage. A pill formulation of the same class is already in clinical trials for age‑related muscle weakness, with Phase 1 data in healthy volunteers reported as safe and active.
Why it matters
- Targets a molecular driver of cartilage loss rather than only treating symptoms, offering a potential disease‑modifying approach.
- If translatable to people, the therapy could reduce the need for joint replacement surgeries caused by osteoarthritis.
- Works by reprogramming existing cartilage cells (chondrocytes), avoiding the complexities of stem‑cell therapies.
- Demonstrated both preventive effects after injury and regeneration in aged tissue, addressing two common routes to osteoarthritis.
Key facts
- The therapy inhibits 15‑PGDH, a protein the authors classify as a 'gerozyme' that increases with age.
- In mouse knee cartilage, 15‑PGDH levels rose roughly two‑fold with age.
- Systemic and intra‑articular administration of a 15‑PGDH inhibitor restored hyaline (articular) cartilage in aged mice.
- After ACL‑like injury, mice given injections twice weekly for four weeks showed greatly reduced progression to osteoarthritis and improved limb use.
- Single‑cell analysis showed one 15‑PGDH‑expressing chondrocyte population fell from 8% to 3% after treatment; fibrocartilage‑associated cells fell from 16% to 8%; hyaline‑producing cells rose from 22% to 42%.
- 15‑PGDH degrades prostaglandin E2; inhibiting the enzyme increases prostaglandin E2 levels, which the team links to regeneration.
- Human knee tissue taken during joint replacement, when treated ex vivo for one week, showed reduced markers of degradation and signs of articular cartilage regeneration.
- The study was led by researchers including Helen Blau and Nidhi Bhutani and is published in Science.
- A pill form of a 15‑PGDH inhibitor is already in clinical trials for muscle weakness; Phase 1 results in healthy volunteers showed the drug to be safe and active.
What to watch next
- Whether clinical trials will begin testing 15‑PGDH inhibitors specifically for osteoarthritis or joint regeneration: not confirmed in the source.
- Long‑term durability and mechanical performance of regenerated cartilage in living animals and humans: not confirmed in the source.
- Safety and side‑effect profile of repeated intra‑articular or systemic dosing in patients with joint disease: not confirmed in the source.
Quick glossary
- 15‑PGDH: An enzyme that breaks down prostaglandin E2; described by the authors as a 'gerozyme' whose levels rise with age and which can limit tissue regeneration.
- Chondrocyte: A specialized cell that makes and maintains cartilage extracellular matrix in joints.
- Hyaline (articular) cartilage: Smooth, glossy cartilage that covers joint surfaces and provides low‑friction movement; commonly lost in osteoarthritis.
- Prostaglandin E2 (PGE2): A signaling lipid involved in inflammation and tissue repair; its levels are regulated in part by 15‑PGDH.
- Gerozyme: A term used by the researchers to describe enzymes that contribute to the aging‑related decline in tissue function.
Reader FAQ
Has this treatment been tested in people?
Human knee tissue treated ex vivo showed regenerative changes, but clinical testing of the therapy for joint disease in patients is not confirmed in the source.
Does the approach use stem cells?
No. The study reports regeneration by changing gene expression in existing chondrocytes rather than recruiting stem or progenitor cells.
Is an oral drug available now for osteoarthritis?
A pill formulation of a 15‑PGDH inhibitor is in clinical trials for age‑related muscle weakness, but availability and trials for osteoarthritis are not confirmed in the source.
Did the treatment prevent arthritis after joint injury?
In mice, a four‑week regimen of injections after an ACL‑like injury substantially reduced progression to osteoarthritis and improved limb function.
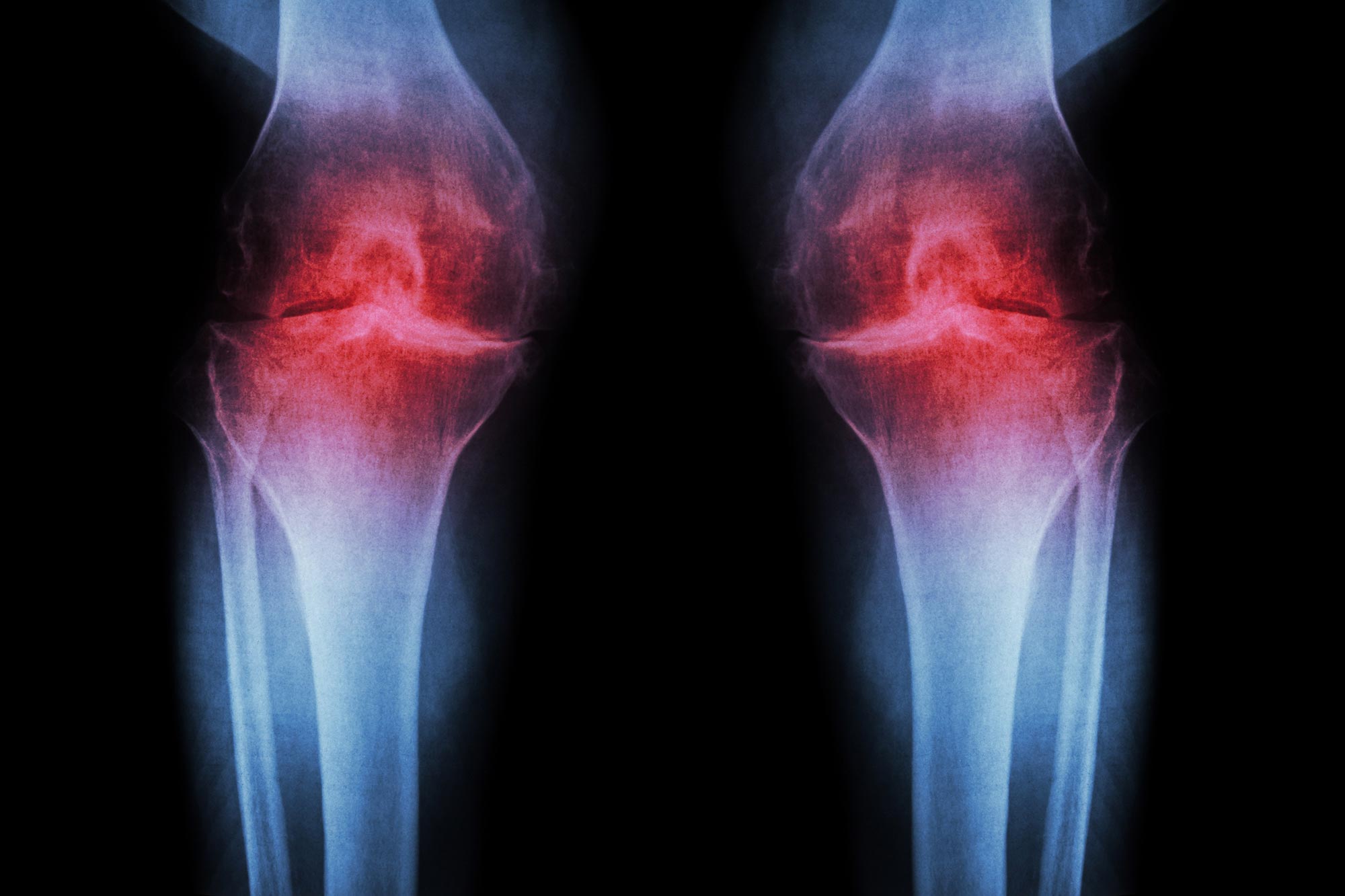
SHARE Scientists have identified a way to regenerate cartilage by targeting a protein that increases with age, reversing joint damage in older animals and preventing arthritis after injury. Credit: Stock…
Sources
- Anti-Aging Injection Regrows Knee Cartilage and Prevents Arthritis
- Inhibiting a master regulator of aging regenerates joint …
- Blocking a master regulator of aging regenerates joint …
- Stanford Researchers Demonstrate Cartilage Regeneration …
Related posts
- Xreal Neo mobile dock blends battery, DisplayPort, and MagSafe design
- Narwal Flow 2 robovac adds AI object tagging to help locate lost items
- Baseus’ new Spacemate RD1 Pro desktop dock includes a Qi2 25W charger